1. Understanding Digestive Enzymes
Digestive enzymes are specialized proteins that play a crucial role in breaking down the food we eat into absorbable nutrients. Without them, our bodies struggle to extract energy and vital compounds from meals, leading to discomfort, nutrient deficiencies, and chronic digestive issues. The three main classes of digestive enzymes include amylases (which digest carbohydrates), proteases (which break down proteins), and lipases (which break down fats). Other important enzymes like lactase, cellulase, and maltase help digest specific food components like dairy sugars, plant fibers, and malt sugar, respectively.
These enzymes are naturally produced by the salivary glands, stomach, pancreas, and small intestine. However, enzyme production can decline due to factors such as aging, stress, certain medications, low stomach acid, or digestive disorders like IBS and leaky gut. When this happens, the body struggles to digest food efficiently—leading to symptoms like bloating, gas, constipation, heartburn, and fatigue.
Taking the best digestive enzymes supplements can help replenish these enzymes, making digestion smoother and more effective. By improving how your body breaks down food, these digestion supplements also support better nutrient absorption, immune function, and even mood. They are a foundational tool for anyone seeking to optimize their digestive health naturally.

2. Why Take Digestive Health Supplements?
In today’s fast-paced world, digestive health is often compromised by poor dietary habits, stress, and environmental toxins. Many women experience symptoms like bloating, indigestion, gas, or food sensitivities but don’t realize that these can be signs of enzyme deficiency. Digestive health supplements, particularly the best digestive enzymes supplements, offer a safe and effective way to support the body’s natural digestive processes and improve gut function.
Digestive enzymes supplements are especially helpful if your body struggles to break down certain foods—such as dairy, fats, proteins, or high-fiber meals. These supplements provide targeted enzyme support to ease digestive strain, reduce discomfort after meals, and help prevent issues like acid reflux, constipation, or nutrient malabsorption. They’re also beneficial for those recovering from antibiotic use, dealing with autoimmune issues, or facing hormonal transitions like postpartum or menopause.
When the body can properly digest food, it absorbs vitamins, minerals, and amino acids more efficiently—supporting everything from energy levels and skin health to immunity and mental clarity. This is why digestion supplements are not just for those with digestive disorders; they’re valuable for anyone aiming to optimize wellness from the inside out. A healthy gut truly lays the foundation for whole-body health.
3. How Digestive Enzymes Work in the Body
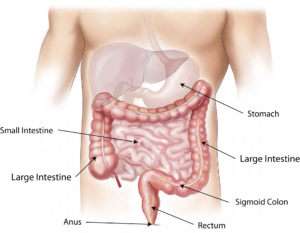
Digestive enzymes are essential for converting complex food molecules into simple, absorbable nutrients. Without them, even the healthiest diet cannot deliver its full benefits. The journey of digestion begins the moment food enters your mouth and continues through your digestive tract, with enzymes playing a central role every step of the way.
3.1 Activation in the Mouth and Stomach
Digestion starts in the mouth where salivary amylase breaks down carbohydrates into simple sugars. As food reaches the stomach, gastric enzymes like pepsin begin breaking down proteins in the acidic environment. Hydrochloric acid (HCl) in the stomach activates these enzymes and provides a sterile, acidic pH needed for protein digestion.
3.2 Small Intestine Enzyme Action
Most digestive enzymes are released from the pancreas into the small intestine. These include proteases, lipase, and amylase, which act on proteins, fats, and carbs respectively. The gallbladder also contributes by secreting bile to emulsify fats, enhancing lipase efficiency. Nutrient absorption occurs primarily in the small intestine, so proper enzymatic breakdown here is critical.
3.3 Enzyme Supplementation
If the pancreas or digestive organs do not produce enough enzymes—due to aging, stress, medical conditions, or hormonal changes—undigested food can lead to bloating, inflammation, and nutrient loss. Supplementing with the best digestive enzymes supplements fills this gap, enabling your digestive system to function more effectively and comfortably.
4. Top 5 Best Digestive Enzymes Supplements
With a growing focus on gut health, the market is flooded with digestion supplements. However, not all are created equal. The best digestive enzymes supplements combine enzyme potency, clean ingredients, and holistic benefits. Below are five standout options that have earned high praise for improving digestion and overall wellness.
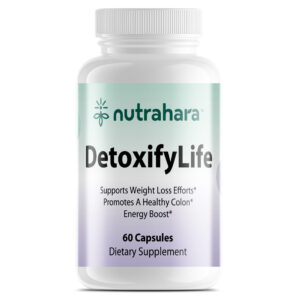
4.1 Nutrahara DetoxifyLife
DetoxifyLife is a powerhouse blend that goes beyond basic digestive enzymes by supporting liver detox, colon cleansing, and gut balance. Infused with key botanicals like milk thistle, cascara sagrada, fennel seed, and aloe vera, this supplement gently stimulates digestion while flushing toxins that hinder enzyme performance. It promotes regular bowel movements, reduces bloating, and preps your gut to absorb nutrients efficiently. It’s ideal for women experiencing sluggish digestion or hormonal changes that disrupt the gut-liver axis.
4.2 Nutrahara FatBlitz
FatBlitz is another standout in Nutrahara’s lineup. While primarily marketed for fat metabolism and weight support, FatBlitz contains digestion-enhancing ingredients such as ginger, cayenne, apple cider vinegar, and green tea extract. These botanicals stimulate bile flow and thermogenic activity, helping the body break down dietary fats more efficiently. This makes it a perfect complement to high-fat meals or ketogenic-style diets where lipase support is critical.
4.3 Garden of Life Organic Digest+
A certified organic formula with 29 powdered fruits and vegetables, this gentle blend is designed for those with sensitive stomachs. It includes enzymes for carbs, fats, and proteins.
4.4 Pure Encapsulations Digestive Enzymes Ultra
Highly rated by healthcare professionals, this medical-grade supplement delivers broad-spectrum enzyme support with a hypoallergenic formula.
4.5 Enzymedica Digest Gold
Backed by extensive enzyme science, Digest Gold offers high-potency enzymes plus ATP to boost energy and digestive power.
5. 7 Tips for Choosing the Best Digestive Enzymes Supplements
With so many digestion supplements on the market, it’s essential to choose the right one tailored to your body’s needs. These expert tips will help you identify the best digestive enzymes supplements for long-term digestive support.
5.1 Choose a Broad-Spectrum Enzyme Formula
Look for a supplement that contains multiple enzymes such as amylase, protease, lipase, lactase, and cellulase. These cover all three macronutrients—carbohydrates, proteins, and fats—as well as specific food components like dairy and fiber.
5.2 Match the Enzymes to Your Diet
If you consume a high-fat diet, prioritize supplements with lipase (such as Nutrahara’s FatBlitz). For protein-heavy meals, make sure protease is included. Digesting complex carbs? Amylase and cellulase are essential.
5.3 Look for Digestive Support Herbs
Botanicals like ginger, turmeric, fennel, cayenne, aloe vera, and milk thistle can naturally soothe the gut and enhance enzyme function. Nutrahara DetoxifyLife is a great example—it combines plant-based enzymes with detoxifying herbs to support the gut-liver connection.
5.4 Avoid Artificial Ingredients
The best digestion supplements are free of fillers, binders, artificial colors, and common allergens like gluten, soy, and dairy. Always check the ingredient list to avoid gut irritants.
5.5 Prefer Plant-Based or Vegan Enzymes
Plant-based enzymes (like bromelain and papain) are easier to digest and often more suitable for sensitive stomachs or individuals avoiding animal-based ingredients.
5.6 Check for Third-Party Testing
Make sure your supplement has been tested for purity, potency, and contaminants. Certifications build trust in quality and transparency.
5.7 Timing Matters: Take With Meals
For maximum benefit, take digestive enzymes with the first bite of food. They work best when present at the start of the digestive process.
6. Digestive Enzymes for Women: Special Considerations
Women experience unique hormonal shifts that significantly influence digestion, nutrient absorption, and gut function. From menstruation and pregnancy to postpartum recovery and menopause, the digestive system often reflects these changes—making digestive health supplements especially vital throughout every life stage.
6.1 During the Menstrual Cycle
Hormonal fluctuations during the menstrual cycle can cause bloating, constipation, or diarrhea due to changing progesterone and estrogen levels. Taking the best digestive enzymes supplements during this time helps regulate bowel movements and reduce water retention and cramping. Herbal-infused formulas like Nutrahara DetoxifyLife, which contain anti-inflammatory and detoxifying botanicals, can provide added support.
6.2 Pregnancy and Lactation
Pregnancy increases the demand for nutrients while slowing digestion due to progesterone. This often leads to indigestion, heartburn, and constipation. Enzyme supplements with gentle ingredients, such as bromelain (from pineapple) and ginger (as found in Nutrahara FatBlitz), can ease digestion without harming the baby. Always consult a healthcare provider before starting any new supplement while pregnant or breastfeeding.
6.3 Postpartum Recovery
The body needs help restoring normal digestive function after childbirth. Hormonal shifts, stress, and sleep deprivation can impair enzyme production. Women recovering from pregnancy may also be dealing with postpartum hair loss, fatigue, or nutrient depletion—issues that are compounded by poor digestion. Enzyme support aids nutrient absorption and gut healing, making it a crucial part of postpartum care.
6.4 Menopause and Aging
As estrogen declines during menopause, so does digestive enzyme production—leading to slower metabolism, bloating, and food sensitivities. Supplementing with a comprehensive digestion supplement restores enzyme levels, supports weight management, and improves nutrient uptake.
By choosing the best digestive enzymes supplements, women can better navigate hormonal transitions and maintain gut wellness throughout all phases of life.
7. Real-Life Testimonials from Women
🧡 1. Emily, 38 – Denver, CO
“After struggling with post-meal bloating for years, I finally tried Nutrahara’s DetoxifyLife. Within a week, I felt a difference—my digestion became more regular, and the uncomfortable bloating was gone. I also noticed better skin and energy levels. It’s now a part of my daily wellness routine.”
🧡 2. Karina, 41 – San Jose, CA
“Perimenopause hit me hard—digestive issues, fatigue, and sudden food intolerances. I switched to FatBlitz by Nutrahara to help with metabolism and digestion. Not only did I notice a reduction in gas and heaviness after meals, but I also shed a few pounds naturally. It’s the best digestive enzyme supplement I’ve tried.”
🧡 3. Meera, 29 – Tampa, FL
“As a vegan, I often felt bloated after eating legumes or fiber-rich meals. A friend recommended a plant-based digestive enzyme blend. After adding one with bromelain, papain, and herbal extracts to my routine, I no longer feel gassy or sluggish. Total game-changer!”
🧡 4. Sandra, 54 – Portland, OR
“During menopause, my digestion slowed down, and I was constantly tired after eating. Nutrahara’s DetoxifyLife helped ease constipation and restored my gut balance. I also appreciate the clean, herbal formula—it’s gentle but effective.”
🧡 5. Priya, 35 – New York, NY
“Between my busy work schedule and raising two kids, I wasn’t digesting meals properly. I’d feel bloated and foggy. Since starting FatBlitz, my digestion is more efficient, and I feel lighter after eating. Plus, it supports fat metabolism, which is a nice bonus!”
8. Conclusion: Restore Digestive Balance Today
Your digestive health is the cornerstone of your overall vitality—affecting everything from energy levels and immunity to mood, skin, and hormonal balance. Whether you’re struggling with bloating, fatigue, food sensitivities, or irregular bowel movements, the right digestion supplements can make a life-changing difference.
Among the wide array of options available today, Nutrahara’s DetoxifyLife and FatBlitz stand out as two of the best digestive enzymes supplements for women. Formulated with plant-based enzymes and fortified with potent herbs, these supplements go beyond basic digestion support. They’re designed with real women’s needs in mind—supporting gut-liver detox, hormone regulation, and nutrient absorption at every life stage.
- DetoxifyLife is ideal for those looking to gently cleanse the digestive tract, reduce inflammation, and restore regularity. Whether you’re navigating hormonal changes, recovering postpartum, or simply feeling off-balance, this blend provides comprehensive gut support rooted in nature.
- FatBlitz is your ally for breaking down fats efficiently, supporting metabolism, and enhancing post-meal comfort. It’s especially effective for women on higher-fat or protein-rich diets, or those struggling with sluggish digestion during perimenopause or menopause.
If you’re ready to take control of your gut health, don’t wait for discomfort to define your day. Rebuild your foundation from within—with clean, clinically-formulated, and plant-powered digestive supplements made for women like you. Trust Nutrahara to help you bridge nature and science for a truly balanced, vibrant life.
✨ Your wellness begins in the gut. Let Nutrahara DetoxifyLife and FatBlitz be your first step to feeling your best—naturally.
Written by the Nutrahara Team
This article was developed by the Nutrahara team of nutrition scientists and naturopaths, who specialize in formulating safe, effective, and science-backed supplements for women’s health. Every ingredient we use is carefully selected to support your body’s unique needs—naturally. Follow us on LinkedIn for expert insights and updates on our latest wellness solutions.