1. Introduction: What Is Brain Fog and Why It Matters
Brain fog is a term used to describe a group of cognitive symptoms that impact your ability to think clearly, focus, and remember details. While not a clinical diagnosis, brain fog can feel very real—especially for women navigating major life transitions like menopause, postpartum recovery, or chronic stress. The experience is often described as feeling mentally “cloudy,” forgetful, slow, or unfocused, even after a full night’s sleep.
For many women, brain fog is triggered by hormonal fluctuations, nutritional deficiencies, or chronic fatigue. Postpartum mothers, in particular, may experience brain fog due to poor sleep, nutrient depletion from breastfeeding, and stress—all of which can compound the challenges of postpartum hair loss treatment. Meanwhile, midlife women entering perimenopause or menopause often report foggy thinking as estrogen levels decline, affecting neurotransmitter activity in the brain.
Thankfully, there are effective ways to address this issue. Natural supplements for brain fog have emerged as safe, targeted tools to support mental clarity and cognitive resilience. These include adaptogens, B-complex vitamins, and amino acids that nourish the nervous system and restore balance. When used alongside proper nutrition and digestion support, these supplements can help lift the fog, sharpen memory, and restore a sense of well-being—especially for women juggling hormonal, emotional, and physical demands.
2. Why Use Supplements for Brain Fog
Brain fog can feel like walking through molasses—words escape you, focus is elusive, and even simple tasks seem overwhelming. While lifestyle factors like sleep, hydration, and stress management are foundational, many women find that targeted supplements for brain fog accelerate their recovery and restore mental clarity more effectively.
These supplements work by addressing common nutrient deficiencies, supporting neurotransmitter production, and enhancing blood flow to the brain. Key ingredients—such as B-vitamins, omega-3 fatty acids, adaptogens like ashwagandha, and magnesium—play crucial roles in cognitive function. When combined, they provide a multifaceted approach to improving memory, reducing anxiety, and boosting mental energy.
Women dealing with postpartum hair loss treatment may be surprised to learn that the same nutrient imbalances causing hair shedding—such as iron, biotin, and collagen deficits—can also affect brain function. In fact, postpartum brain fog is often worsened by these deficiencies. Incorporating digestion-friendly, bioavailable supplements not only supports hair regrowth but also enhances clarity and cognitive performance.
Additionally, Nutrahara’s line of brain support supplements—including FocusZenith, RestoraSleep, AnxioGuard, and Ashwagandha with Black Pepper—are designed to provide safe, plant-based support for women at all stages of life. These formulas help women regain control over their focus, productivity, and overall mental wellness.
3. Best Supplements for Brain Fog: Natural Solutions That Work
3.1 FocusZenith
FocusZenith is Nutrahara’s signature brain health formula designed for women seeking mental clarity, sharper memory, and sustained focus. This plant-powered supplement contains a precise blend of B-complex vitamins, ginkgo biloba, bacopa monnieri, and adaptogens that enhance neural communication and protect against cognitive decline.
One of the primary causes of brain fog in women—especially during menopause or postpartum recovery—is the depletion of neurotransmitters due to hormonal shifts. FocusZenith works by replenishing those essential nutrients, supporting the brain’s energy systems, and promoting cerebral circulation.
It is particularly effective for professionals and mothers who struggle with daily brain fatigue, as it enhances focus without relying on stimulants. Additionally, the adaptogens in FocusZenith help reduce cortisol levels, making it beneficial for women experiencing mental fog due to stress or burnout. When used alongside postpartum recovery plans or postpartum hair loss treatment, this supplement helps restore both cognitive and emotional balance.
If you’re looking for comprehensive supplements for brain fog that support both short-term focus and long-term brain health, FocusZenith offers a synergistic solution grounded in science and inspired by nature.
3.2 RestoraSleep
Sleep and cognitive health go hand in hand. Without restful, uninterrupted sleep, the brain cannot detoxify or regenerate properly. That’s where RestoraSleep comes in—Nutrahara’s nighttime formula that supports deep sleep, hormonal balance, and neural recovery.
Formulated with natural ingredients like L-theanine, melatonin, valerian root, and passionflower, RestoraSleep helps calm the nervous system, balance the circadian rhythm, and ensure the body enters the deep sleep stages essential for memory consolidation and emotional regulation.
This supplement is especially powerful for women dealing with postpartum insomnia or menopausal sleep disruptions. In both cases, the resulting fatigue can intensify brain fog symptoms. As a companion to postpartum hair loss treatment, RestoraSleep works synergistically by supporting the hormonal and neurological systems affected after childbirth.
Lack of quality sleep is one of the most overlooked contributors to brain fog. By enhancing your nighttime recovery, RestoraSleep sets the foundation for better focus, clarity, and productivity during the day—making it a core part of any supplements for brain fog routine.
3.3 AnxioGuard
Chronic stress and anxiety are two of the most common underlying causes of brain fog in women. AnxioGuard is Nutrahara’s advanced calming formula designed to reduce nervous system overload and promote mental calm without causing drowsiness or dependency.
This supplement includes clinically studied adaptogens and herbal extracts such as ashwagandha, lemon balm, and passionflower—all known to help reduce cortisol levels and soothe the mind. When stress is reduced, cognitive resources are freed up, allowing for sharper focus, better memory, and improved mood stability.
AnxioGuard is ideal for women juggling careers, caregiving roles, and personal stressors. It’s particularly helpful for new mothers managing hormonal changes and sleep deprivation, two factors that also influence postpartum hair loss treatment effectiveness. By reducing anxiety, AnxioGuard supports overall hormonal harmony, making it a powerful ally in reducing both physical and mental symptoms.
Used consistently, AnxioGuard enhances the performance of other supplements for brain fog by stabilizing the emotional and physiological factors that impair cognition.
3.4 Ashwagandha with Black Pepper
Ashwagandha is a revered adaptogen in Ayurvedic medicine, and Nutrahara’s Ashwagandha with Black Pepper offers a highly bioavailable form for maximum stress-relief and cognitive support. The black pepper extract enhances absorption, ensuring that this supplement delivers fast and lasting benefits.
Ashwagandha helps regulate cortisol, the body’s main stress hormone, which—when chronically elevated—can damage brain cells, disrupt sleep, and worsen mood. By restoring balance to the HPA (hypothalamic-pituitary-adrenal) axis, this supplement supports cognitive clarity, emotional resilience, and better decision-making.
For women navigating menopause, postpartum recovery, or even intense periods of work-related burnout, Ashwagandha is one of the most reliable supplements for brain fog. It not only helps restore mental calm but also improves energy levels and mood stability. Women undergoing postpartum hair loss treatment may find additional benefit in Ashwagandha’s adaptogenic effects, as it supports hormonal equilibrium and reduces inflammation.
Whether taken alone or in combination with FocusZenith or AnxioGuard, Nutrahara’s Ashwagandha supplement is a natural powerhouse that helps clear the fog—gently and effectively.
4. Best Supplements for Menopause Brain Fog
4.1 Hormonal Changes and Cognitive Decline
As women enter perimenopause and menopause, shifting hormones—especially declining estrogen levels—can significantly impact cognitive function. Estrogen is essential for maintaining brain plasticity, mood regulation, and verbal memory. When levels drop, many women report increased forgetfulness, poor concentration, and difficulty processing information. This phenomenon, commonly referred to as “menopause brain fog,” can last for months or even years if left unaddressed.
Other symptoms such as night sweats, sleep disturbances, and anxiety often compound the issue, further reducing mental clarity and increasing emotional strain. While many women turn to lifestyle changes or hormone replacement therapy, others are turning to natural supplements for brain fog that specifically support cognitive and hormonal balance during this life phase.
Although menopause and postpartum are distinct stages, both involve drastic hormonal transitions and share some similar symptoms. Interestingly, some ingredients used in postpartum hair loss treatment—like collagen, iron, and adaptogens—also support mental wellness during menopause.
4.2 Nutrahara Solutions for Menopause Brain Fog
Nutrahara offers targeted herbal and nutritional solutions to help menopausal women regain clarity, calm, and cognitive stamina. The following supplements are especially effective:
- FocusZenith: A daily cognitive booster formulated with brain-essential nutrients like B-complex vitamins and ginkgo biloba. It helps enhance focus, alertness, and memory—especially useful for women facing menopause-related mental dips.
- Ashwagandha with Black Pepper: An adaptogen that naturally lowers cortisol levels and supports hormonal balance, making it ideal for counteracting menopause-induced stress and forgetfulness.
- AnxioGuard: This calming blend reduces anxiety, stabilizes mood, and promotes mental resilience—perfect for easing emotional turbulence that accompanies hormonal fluctuations.
Together, these supplements for brain fog work synergistically to help women navigate the cognitive and emotional challenges of menopause with confidence and clarity.
5. Supplements for Brain Fog During Postpartum Recovery
5.1 Postpartum Cognitive Fatigue
Postpartum is a beautiful yet demanding chapter of life. As a new mother navigates the emotional rollercoaster, hormonal changes, and chronic sleep deprivation that follow childbirth, she may also face unexpected cognitive symptoms—commonly referred to as “mommy brain” or postpartum brain fog.
This form of brain fog is marked by forgetfulness, difficulty focusing, and slower information processing. For many women, these issues are exacerbated by iron deficiency, thyroid fluctuations, and nutrient depletion from breastfeeding. Additionally, women undergoing postpartum hair loss treatment may be unaware that the very deficiencies contributing to hair thinning—like low levels of iron, B-vitamins, and collagen—can also impair mental clarity.
Postpartum women need gentle, non-stimulant solutions that support mental clarity, hormonal balance, and emotional resilience without disrupting breastfeeding or sensitive recovery phases. That’s where supplements for brain fog formulated for this life stage become invaluable.
5.2 Nutrahara Recommendations for Postpartum Brain Fog
Nutrahara’s women-first approach provides safe, plant-based solutions designed specifically to nourish postpartum brains:
- RestoraSleep: Sleep is foundational for postpartum recovery and brain detoxification. RestoraSleep promotes deeper, more restorative sleep with non-habit-forming herbs like valerian root and passionflower—making it ideal for new moms battling brain fog and exhaustion.
- Ashwagandha with Black Pepper: As a natural adaptogen, Ashwagandha helps stabilize mood, reduce anxiety, and balance cortisol levels during this emotionally intense period. It supports both mental clarity and hormonal recovery.
- FocusZenith: When you’re ready to return to work or tackle everyday tasks with more clarity, FocusZenith offers safe cognitive support. Its blend of B-vitamins, nootropics, and botanicals helps improve focus, recall, and productivity—even amid sleep-deprived chaos.
These supplements for brain fog can be paired with nutrient-dense postpartum hair loss treatments to form a holistic recovery routine. By addressing both visible and invisible symptoms of postpartum depletion, women can feel mentally sharp, emotionally balanced, and physically empowered as they transition into motherhood.
6. Real-Life Testimonials from Women
Hearing from real women who’ve overcome brain fog using targeted wellness solutions can be incredibly inspiring. Below are five powerful stories from women at different life stages—each finding mental clarity through Nutrahara’s supplements for brain fog, digestive health supplements, and holistic health practices.
Emily R., 42 – San Diego, CA (Perimenopausal Brain Fog)
“Brain fog hit me hard in my early 40s. I’d forget why I walked into a room, lose focus during work meetings, and constantly misplace things. A friend suggested I try Nutrahara’s FocusZenith along with AnxioGuard. Within two weeks, I felt clearer, calmer, and finally back in control. Adding DetoxifyLife also improved my digestion—and surprisingly, my energy levels too!”
Jessica T., 34 – Austin, TX (Postpartum Recovery)
“After my second baby, I was dealing with severe brain fog and hair loss. My doctor recommended iron and collagen, but what made the biggest difference was the Nutrahara stack: RestoraSleep helped me sleep deeply, and Ashwagandha kept me emotionally steady. I paired it with their postpartum hair loss treatment routine and I feel more like myself than I have in months.”
Samantha L., 29 – New York, NY (New Mom & Entrepreneur)
“Juggling a newborn and my business left me completely fogged out—no memory, no energy, no patience. FocusZenith in the morning and RestoraSleep at night turned things around quickly. I even started using FatBlitz to support digestion, which surprisingly helped me absorb nutrients better and stabilize my mood. Highly recommend it to all busy moms!”
Karen M., 56 – Denver, CO (Menopause + Digestive Issues)
“I assumed brain fog was just part of aging, but it was affecting my quality of life. I found Nutrahara while researching digestion supplements and decided to try both their brain and gut support. Within 30 days of using AnxioGuard, FocusZenith, and DetoxifyLife, I felt mentally sharper and had less bloating. A total win.”
Deepa S., 48 – Fremont, CA (Stress-Related Brain Fog)
“As a working mom caring for aging parents, my stress levels were through the roof. I couldn’t think clearly, and it was affecting my confidence. Nutrahara’s Ashwagandha with Black Pepper and AnxioGuard gave me back my balance. I combined them with digestion supplements and noticed that once my gut felt better, my brain did too. I finally feel focused again.”
7. Conclusion: A Clearer Mind Starts from Within
Brain fog can feel frustrating, debilitating, and disorienting—but it is not permanent. By identifying the root causes—whether hormonal shifts, stress, poor sleep, gut imbalance, or nutrient deficiencies—women can take empowered steps toward mental clarity.
Natural supplements for brain fog are powerful tools when used as part of a broader wellness routine. Nutrahara’s women-focused solutions, including FocusZenith, RestoraSleep, AnxioGuard, and Ashwagandha with Black Pepper, offer comprehensive cognitive and emotional support across every life stage—from postpartum recovery to menopause and beyond.
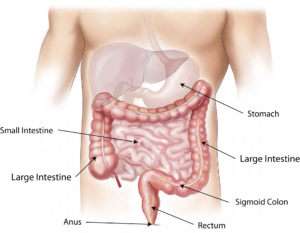
Equally important is nurturing the gut. Without proper digestion and nutrient absorption, even the best brain supplements won’t reach their full potential. That’s why combining cognitive support with digestive health supplements like DetoxifyLife and FatBlitz delivers lasting results—clearing both your mind and your body.
If you’re also undergoing postpartum hair loss treatment, the same nutrients that nourish your scalp and skin often benefit your mood, memory, and focus. When your body heals from the inside out, your mind follows.
Incorporate these targeted strategies and products into your daily routine, and you’ll not only conquer brain fog—you’ll feel sharper, stronger, and more grounded than ever.